What is United Kingdom Ulcerative Colitis Industry?
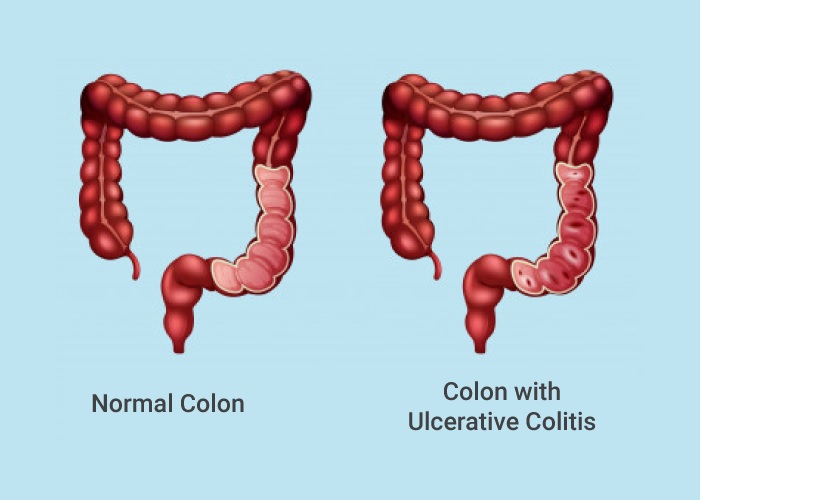
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in the lining of the large intestine (colon) and rectum. The exact cause of UC is unknown, but it is believed to be an autoimmune disease where the immune system attacks healthy cells in the colon, causing inflammation and sores. Symptoms of active disease include abdominal cramping, diarrhea, rectal bleeding, fever, and weight loss. The condition usually starts in the rectum and lower colon but can sometimes extend through the entire colon.
Symptoms and Diagnosis
The main symptoms of Ulcerative Colitis typically include abdominal pain and cramping, diarrhea (which may be bloody), rectal bleeding, and weight loss. Diarrhea is usually the first symptom, which is often bloody in nature. Fatigue is also common. The frequency and severity of symptoms can vary significantly between individuals and even for the same person over time. For some people symptoms may come and go in episodes or “flares” while others have nearly continuous symptoms.
Doctors use a combination of exams, medical history, and tests to diagnose UC. A physical exam can reveal tenderness, inflammation, or masses in the abdomen. During a rectal exam the doctor may see mucosal changes, small sores, or bleeding in the rectum and lower colon. Blood tests can show anemia or a high white blood cell count indicating inflammation. Stool tests may detect blood or signs of infection. A colonoscopy, which uses a tiny camera on a flexible tube inserted through the rectum, provides the most definitive view of the inside of the colon and evidence of ulcers or inflammation. During the procedure a tiny sample of colon tissue (biopsy) may also be taken to confirm diagnosis under a microscope. Other tests like CT scans or MRI may occasionally be used to help diagnosis or rule out other conditions.
Treatment and Management
There is currently no cure for ulcerative colitis, but various treatment options exist to help control symptoms and periods of inflammation or flare-ups. The main goals of treatment are to induce and maintain remission, improve quality of life, and prevent complications like colon cancer that may develop over time. Treatment plans are tailored to the individual based on factors like severity and location of disease in the colon. Mild cases are typically treated with oral medications like 5-ASAs, corticosteroids like prednisone, or immunomodulators like azathioprine. For moderate to severe cases, biologic therapies that target specific parts of the immune system like infliximab or adalimumab may be added or used instead.
Some people may need surgery to remove the colon if medical treatment is not effective or to prevent cancer. Types of surgery include colectomy with ileostomy or restorative proctocolectomy with ileal pouch-anal anastomosis. Following surgery, the goal is to maintain wellness through diet, exercise, stress management, and medications to prevent disease recurrence. Close monitoring by a gastroenterologist is also important, particularly after surgery, to check for flare-ups or complications. Proper nutrition, staying hydrated, not smoking, immunizations, and cancer screenings can help improve outcomes as well.
Mental Health Challenges
Having a chronic condition like ulcerative colitis can take a significant mental and emotional toll. Not only does the disease often cause unpleasant physical symptoms, but it requires ongoing medical management and lifestyle changes. Issues like unpredictability of flare-ups, pain, fatigue, loss of control over one’s body, disruptions to daily life, body image concerns, work/school absences, fear of surgery, relationship difficulties, and worries about cancer risks can all contribute to higher rates of depression, anxiety, and stress.
A 2016 survey by Crohn’s and Colitis UK found that nearly 60% of people with IBD in the UK report feeling depressed about their condition and over 70%experience anxiety. Younger people under 30 may be especially prone to psychological distress from IBD. Coping with a chronic disease at a formative life stage brings additional challenges. Social isolation, embarrassment over symptoms, and concerns about relationships and fertility are common among younger patients. Support groups and mental health counseling can help people effectively manage the psychological aspects of ulcerative colitis. Physicians also need to be aware of mental health issues and incorporate screening into routine care.
Impact on Daily Life United Kingdom Ulcerative Colitis Industry
Ulcerative colitis significantly impacts quality of life for many patients. Unpredictable flare-ups mean living with the constant fear of symptoms suddenly worsening, often with little warning. The very real physical limitations from pain, fatigue, frequent diarrhea or bleeding can restrict independent living, activities, travel, and social interactions. Sleep deprivation from nocturnal trips to the bathroom further perpetuates the cycle of fatigue. Maintaining employment or education likewise poses difficulties. Job performance and attendance may suffer during active periods requiring extended sick leave. Heavy or physically demanding roles may necessitate finding alternative work.
According to the 2016 UK IBD Audit, over 20% of patients reported having to reduce work hours or change jobs and as many as 14% claimed they were unemployed due to their condition. Fear of discrimination or job loss discourages many from divulging the nature of their illness to employers. The financial burden from medical costs not fully covered by the NHS also mounts additional stress. While the right workplace accommodations, understanding from employers and supportive sick policies provide relief, ulcerative colitis intrudes significantly on education, careers and pursuits for a large subset of those living with the illness in the UK.
Rising Incidence and Economic Burden
The prevalence and incidence rates of ulcerative colitis in the UK have been steadily increasing with the last few decades, echoed globally. Genetic and environmental changes likely partly account for this upward trend. Estimates suggest the total number of UC cases in the UK exceeds 240,000. Due to its chronic recurring nature, UC carries substantial personal, health system and societal costs. Between 2011-2012 the annual direct costs to the NHS for all IBD topped £983 million and a 2018 study estimated the total societal burden was over £2.35 billion factoring in indirect costs like lost productivity. Average yearly treatment costs per UC patient range from £2,500-5,000 based on severity and management approach, with hospitalizations and surgery exponentially raising this figure.
As standards of care, available medications and need for lifelong monitoring advance, the economic impact continues growing. Cutbacks in NHS funding have exacerbated challenges meeting demand. Though some biologic therapies receive national approval, timely access varies regionally. Out-of-pocket costs pressure many. More research is urgently needed into both more effective, affordable treatment models and preventive strategies targeting the rising incidence of UC in the UK. Economic ramifications highlight the substantial resources devoted to managing this chronic inflammatory bowel condition.
Overall, despite the significant number of individuals affected, the report highlights the challenges in diagnosing UC, with an average diagnostic delay of 12 years in some cases. The primary reason for this delay is the non-specific nature of symptoms, which can be mistaken for other conditions.
*Note:
1.Source: CoherentMI, Public sources, Desk research
2.We have leveraged AI tools to mine information and compile it