A team of researchers led by UT Southwestern Medical Center has published a retrospective study in Nature Cancer that challenges the long-held belief that the number of mutations in cancerous tumors is an indicator of how effectively patients will respond to immune checkpoint inhibitors (ICIs).
The study, which upends conventional wisdom, could lead to more precise methods for determining which patients will benefit most from this type of immunotherapy. Dr. David Hsieh, M.D., Assistant Professor of Internal Medicine in the Division of Hematology and Oncology and a member of the Harold C. Simmons Comprehensive Cancer Center at UT Southwestern, served as the study’s leader.
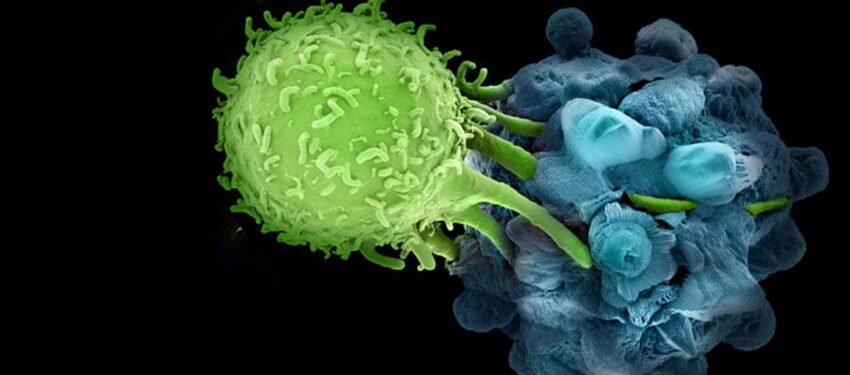
ICIs have transformed cancer therapy since the first drug in this category was approved by the U.S. Food and Drug Administration in 2011. Since then, seven other ICIs have entered the U.S. market, all working by blocking protein checkpoints that prevent the immune system from attacking cancer cells. While ICIs have the potential to significantly extend survival, clinical trials have shown that they are effective for only a fraction of patients. The number of mutations present in cancer cells has been considered a reliable predictor of ICI success.
For instance, pembrolizumab, a commonly prescribed ICI for various cancers such as melanoma, non-small cell lung cancer, and renal cell carcinoma, is approved for patients with tumors containing 10 or more mutations per million base pairs of DNA and whose cancers have progressed on standard treatments.
However, Dr. Hsieh noted that the assumption that tumor mutational burden (TMB) is a consistent marker of ICI effectiveness could be flawed. The studies used to support this idea were relatively small and focused on a limited number of cancer types. Furthermore, the cutoff of 10 or more mutations used to prescribe pembrolizumab was based on weak evidence.
The researchers analyzed data from over 1,000 patients with various types of advanced cancers who had received ICIs. They found that TMB was not a reliable predictor of response to immunotherapy. Instead, they identified other factors, such as the presence of specific mutations and the immune microenvironment, that could better predict treatment success.
These findings could lead to more precise methods for determining which patients will benefit most from ICIs, potentially reducing both undertreatment and overtreatment. Dr. Hsieh emphasized, “Our study challenges the paradigm that tumor mutational burden is a universal marker of how immunogenic a cancer will be. Current standards that rely on this assumption could lead to both undertreatment and overtreatment of patients.”
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it.