What are CAR T cells?
CAR T cell therapy explained
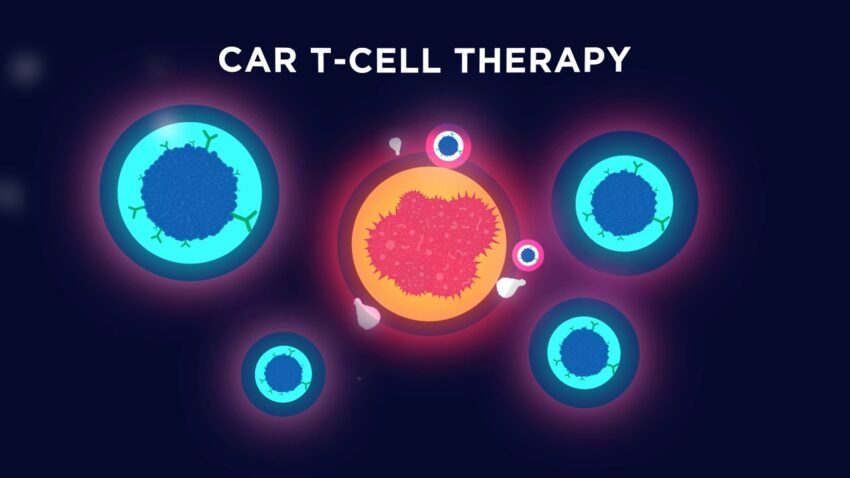
CAR T cell therapy, also called chimeric antigen receptor T cell therapy, is an immunotherapy that uses modified T cells to treat certain types of cancers. In this therapy, T cells are collected from a patient’s blood. The genes that encode a chimeric antigen receptor (CAR) are then introduced into the T cells, which allows the T cells to recognize and attack cancer cells.
The CAR replaces the natural T Cell Receptors (TCRs) on the surface of the T cells with an artificial receptor. This CAR redirects the T cells to recognize and kill cancer cells expressing the target antigen, regardless of the way antigens are normally processed and presented. The most common CAR T cell therapies currently target CD19 antigen, which is highly expressed on B-cell malignancies such as acute lymphoblastic leukemia (ALL) and B-cell non-Hodgkin lymphoma (NHL).
How does it work?
The first step involves extracting T cells from a patient’s blood through leukapheresis. The extracted T cells are then engineered in the laboratory to express a CAR on their surface by transferring the CAR gene into the T cells using a harmless virus. Once the CAR T cells are expanded in number in the laboratory, they are infused back into the patient.
Once re-infused, the CAR T cells recognize the specific protein or antigen on tumor cells. The binding of the CAR triggers the T cells to activate and proliferate in the body. The activated CAR T cells become the body’s “living drugs” and seek out and destroy cancer cells that express the target antigen. By recognizing antigens on cancer cells that the native immune system cannot, CAR T cells can eliminate cancer that has evaded the natural immune response.
Potential benefits of CAR T cell therapy
CAR T cell therapy provides a potentially curative treatment option for certain blood cancers that have not responded to other therapies. Some key potential benefits of CAR T cell therapy include:
– High response rates: Studies have shown response rates over 80% for some blood cancers, including complete remissions in a significant number of patients. These responses have lasted for years in some cases.
– Minimal side effects compared to chemotherapy and radiation: While CAR T cell therapy can cause short-term side effects as the immune system responds, it avoids the long-term side effects of conventional cancer treatments like chemotherapy and radiation which damage healthy cells.
– Durable responses: Researchers have found that some patients who achieve complete remission following CAR T cell therapy remained cancer-free for many years without additional treatment.
– Personalized treatment: As CAR T cells are made from a patient’s own immune cells, there is little risk of major tissue rejection issues compared to organ transplants. It’s a highly personalized treatment tailored to each individual.
– Cost-effective therapy: Compared to a lifetime of costly cancer drugs, one-time CAR T cell therapy has the potential to provide long-term remission in a highly cost-effective manner.
Potential challenges and risks
While promising, CAR T cell therapy is still an evolving treatment approach and faces some challenges:
– Production challenges: Manufacturing individualized CAR T cell treatments for each patient is complex and expensive, requiring specialized facilities. Large-scale production needs to be optimized.
– Toxicity risks: A small proportion of patients receiving CAR T cell therapies experience potentially life-threatening side effects like Cytokine Release Syndrome or neurotoxicity due to an excessive immune response. Careful patient selection and monitoring is important.
– Limited to blood cancers so far: Most success has been seen for blood cancers that express CD19 like ALL and NHL. Applying CAR T therapies for solid tumors presents greater manufacturing and efficacy challenges due to the heterogeneous nature of solid tumors.
– Relapse risk: While remission can last for years, some patients still experience relapses as cancer cells develop ways to evade the CAR T cells over time. Combination therapies may help overcome resistance.
– Individual variability in response: Not all patients see the same levels of response to CAR T therapy. Patient characteristics like fitness level and disease burden impact outcomes.
The future of CAR T cell therapy
Despite current limitations, CAR T cell therapy holds immense potential as a breakthrough cancer treatment. Continued research is helping address the challenges and make this therapy more widely available. Some areas researchers are actively exploring include:
– Developing “armored” CAR T cells enhanced with additional genes to overcome tumor evasion mechanisms.
– Combining CAR T cells with other immunotherapies like checkpoint inhibitors for synergistic effects.
– Engineering “universal” CAR T cells that can target multiple tumor antigens for broader application against cancers.
– Newer CAR designs and targets to expand its use against solid tumors which are more challenging to treat.
– Using CAR T cells earlier in treatment plan or after stem cell transplants to improve outcomes.
– Addressing safety issues through better patient selection criteria and toxicity risk-management strategies.
With ongoing clinical trials evaluating newer generations of CAR T cells and combination strategies, this novel form of immunotherapy is positioned to transform cancer treatment in the years to come.