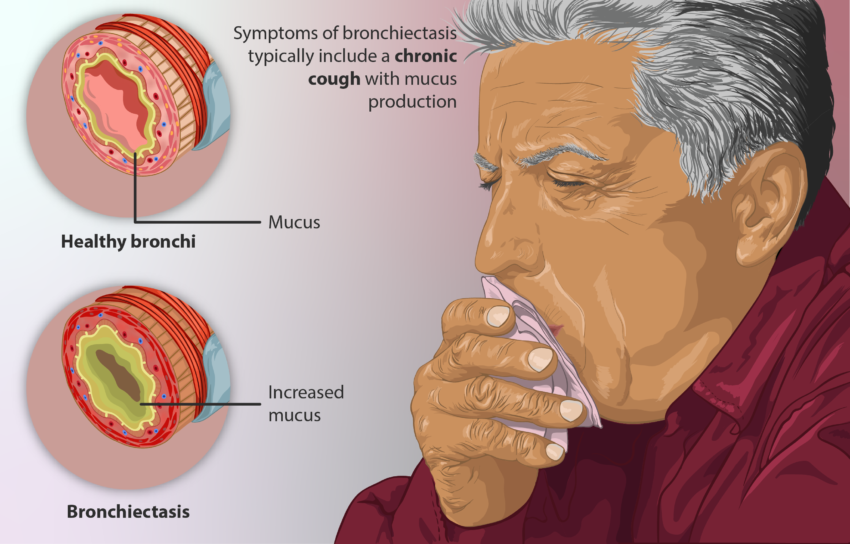
Bronchiectasis is a chronic lung condition characterized by abnormal dilatation of the bronchi and bronchioles. It occurs when the airways of the lungs become damaged or destroyed, allowing them to widen abnormally. This makes it difficult to clear mucus and other debris from the lungs, leading to infections. While there is no cure for bronchiectasis, several drugs are available to manage its symptoms and prevent complications. This article provides an overview of the different classes of drugs used to treat bronchiectasis.
Antibiotics
Antibiotics are the mainstay of treatment for bronchiectasis as bacterial infections often exacerbate symptoms. They are prescribed to treat acute exacerbations as well as prevent recurrent infections.
Oral antibiotics: For mild to moderate symptoms or stable disease, oral antibiotics like amoxicillin, doxycycline and ciprofloxacin are generally sufficient. They are prescribed for 6-8 weeks during an acute exacerbation and may also be taken chronically for disease control.
Intravenous antibiotics: Severe exacerbations requiring hospitalization are treated with intravenous antibiotics like ceftazidime, piperacillin-tazobactam or meropenem. IV antibiotics achieve higher lung concentrations and a faster response. They are administered alone or in combination for 10-14 days.
Inhaled antibiotics: Inhaled antibiotics consisting of colistimethate sodium (colistin) or tobramycin directly target the lungs, achieving high local concentrations with fewer side effects. They are used long-term to prevent exacerbations in patients with frequent infections.
mucolytics
Mucolytic drugs aid in clearing excess mucus from the lungs. They work by reducing the viscosity and elasticity of respiratory mucus secretions, allowing for easier coughing and expectoration. Commonly prescribed mucolytics include:
Hypertonic saline: An inhaled 3% saline solution thins mucus by drawing water into the airways through osmosis. It is the frontline treatment and can reduce exacerbation frequency when used regularly.
DNAse enzymes: Dornase alfa (Pulmozyme) is a recombinant human DNase enzyme that breaks down DNA released during inflammation into smaller, less viscous fragments. It works in combination with chest physiotherapy.
Guaifenesin: An expectorant, it works by stimulating respiratory tract secretions and reducing their viscosity. However, its effectiveness in bronchiectasis is unclear.
Anti-Inflammatory drugs
Bronchiectasis involves chronic inflammation in the airways which contributes to ongoing lung damage over time. Anti-inflammatory drugs may help reduce inflammation and slow disease progression.
Inhaled corticosteroids: Drugs like fluticasone or beclomethasone reduce inflammation in the small airways when used long-term. They are effective in reducing exacerbation frequency but their role in improving lung function is uncertain.
Macrolides: Long-term, low dose macrolides like azithromycin have anti-inflammatory properties apart from antibacterial effects. Regular use can decrease exacerbations and improve quality of life in bronchiectasis, though resistance is a concern.
Immunomodulators: Limited evidence suggests medications modifying immune response like methotrexate or hydroxychloroquine may benefit patients with predominant systemic inflammation and autoimmune diseases like rheumatoid arthritis leading to bronchiectasis. However, more research is still needed regarding their routine use.
Bronchodilators
Bronchodilators are used in bronchiectasis patients who also display bronchospasm, which means reversible narrowing or constriction of the airways. They help relieve symptoms by relaxing and widening the bronchial tubes.
Short-acting beta2-agonists: Drugs like salbutamol are prescribed as relief medication via metered dose inhaler to be used as needed for coughing, wheezing or breathlessness.
Long-acting beta2-agonists: Formoterol or salmeterol provide bronchodilation for 12 hours and are taken twice daily for regular bronchospasm control.
Anticholinergics: Ipratropium bromide acts via a different mechanism from beta-agonists. It provides additive benefits when used along with short-acting beta2-agonists.
Surgery
For a small subset of patients with localized disease, lobectomy (removing an entire lung lobe) or lung volume reduction surgery may be required if drug treatments fail to adequately control complications. These surgical procedures aim to remove the most diseased parts of the lung and improve lung function. They are usually only considered in severe refractory cases on the advice of a respiratory specialist.
Combination Therapies
A multimodal treatment approach using two or more drug classes together is often needed for optimum management of bronchiectasis. Common combinations prescribed include an antibiotic along with an airway clearance technique, a macrolide with inhaled corticosteroid, or a bronchodilator with an anti-inflammatory. Careful monitoring is required to balance maximizing benefits with potential drug interactions and side effects.
In summary, bronchiectasis poses a significant treatment challenge due to its chronic nature and multiple comorbidities. A personalized regimen combining antibiotics, airway clearance measures, mucolytics and anti-inflammatory or bronchodilator therapy tailored to the individual patient’s disease severity and phenotype offers the best approach. Newer targeted biologics also hold promise, but further research is still ongoing. With close medical supervision, the right combination of medicines can help achieve effective symptom management in bronchiectasis.